- Research
- Open access
- Published:
Quantitative data collection approaches in subject-reported oral health research: a scoping review
BMC Oral Health volume 22, Article number: 435 (2022)
Abstract
Background
This scoping review reports on studies that collect survey data using quantitative research to measure self-reported oral health status outcome measures. The objective of this review is to categorize measures used to evaluate self-reported oral health status and oral health quality of life used in surveys of general populations.
Methods
The review is guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) with the search on four online bibliographic databases. The criteria include (1) peer-reviewed articles, (2) papers published between 2011 and 2021, (3) only studies using quantitative methods, and (4) containing outcome measures of self-assessed oral health status, and/or oral health-related quality of life. All survey data collection methods are assessed and papers whose methods employ newer technological approaches are also identified.
Results
Of the 2981 unduplicated papers, 239 meet the eligibility criteria. Half of the papers use impact scores such as the OHIP-14; 10% use functional measures, such as the GOHAI, and 26% use two or more measures while 8% use rating scales of oral health status. The review identifies four data collection methods: in-person, mail-in, Internet-based, and telephone surveys. Most (86%) employ in-person surveys, and 39% are conducted in Asia-Pacific and Middle East countries with 8% in North America. Sixty-six percent of the studies recruit participants directly from clinics and schools, where the surveys were carried out. The top three sampling methods are convenience sampling (52%), simple random sampling (12%), and stratified sampling (12%). Among the four data collection methods, in-person surveys have the highest response rate (91%), while the lowest response rate occurs in Internet-based surveys (37%). Telephone surveys are used to cover a wider population compared to other data collection methods. There are two noteworthy approaches: 1) sample selection where researchers employ different platforms to access subjects, and 2) mode of interaction with subjects, with the use of computers to collect self-reported data.
Conclusion
The study provides an assessment of oral health outcome measures, including subject-reported oral health status and notes newly emerging computer technological approaches recently used in surveys conducted on general populations. These newer applications, though rarely used, hold promise for both researchers and the various populations that use or need oral health care.
Background
A fundamentally different approach is currently needed to address the oral health of populations worldwide namely by considering the perspective of patients or populations and not only dental professionals' views [1]. It seems increasingly necessary to integrate the self-reported perceptions of oral health, as they can complete or even replace clinical measures of dental status in surveys of populations. Indeed, such subjective measures are easy to use in large-scale populations and can provide a broader health perspective as compared to clinically determined measures of dental status alone [2, 3]. Since the topic is broad, this scoping review sets out to identify methods employed in population surveys that discussed self-reported perceptions of oral health, and the extent to which new computer-oriented technological approaches are being incorporated in the research methods.
The literature on oral health and dental-related scoping and systematic reviews includes studies that use specific populations in terms of disease or clinical conditions, treatments, political or social status and typically do not explore oral health status outcome measures [4,5,6,7,8,9,10,11,12,13,14,15]. These studies only occasionally provide perspectives on general populations. A review by Mittal et al. identifies dental Patient-Reported Outcomes (dPROs), and dental Patient Reported Outcome Measures (dPROMs) related to oral function, oral-facial pain, orofacial pain and psychosocial impact [16]. The study affords a valuable and extensive review of self-reported oral health and quality of life measures, many of which are found in this paper. This scoping review, then, seeks approaches used in subject-reported surveys, including those with general populations, which may broaden the perspective on oral health outcome measures.
The objective of this review is to categorize measures used to evaluate self-reported oral health status and oral health quality of life used in surveys of general populations.
Methods
This work is implemented following the framework of scoping reviews [17,18,19] and is presented according to the recommendations of the Preferred Reporting of Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR), as listed in Additional file 1: Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist [20]. Additional file 5: Glossary of Terms provides definitions for the important terms used across the paper.
Search strategy and data sources
A health science librarian assisted in the development of a search strategy that identified papers concerning subject-reported oral health status surveys. The search terms consisted of three broad categories, including survey methods, subject-reported outcomes, and oral health and disease (see Additional file 2: Search Terms for the full list of search strings). The search comprised peer-reviewed journal articles, conference proceedings and reviews with at least one keyword from each of three aspects. Four online databases: Ovid Medline, Embase, Web of Science, and Cochrane Reviews and Trials were used. In addition, a manual search used similar keywords for the gray literature achieved on MedRxiv. The search focused on peer-reviewed papers written in English and published between 2011 to September 2021. Publications in the last decade were reviewed to investigate the extent to which different methods were being used and the trends that occurred during this period. The final search was completed on September 29, 2021. Using the current decade provides a period where there is considerable interest in non-clinical oral health status outcome measures and the potential for examining technological innovation. All references were imported for review and appraisal. Duplicates were identified using Mendeley (Mendeley, London, UK) and manually verified. After removing the duplicates, data were tabulated in Microsoft Excel (Microsoft, Redmond, WA, USA) for recording screening results and data charting.
Study inclusion criteria
Studies that did not meet with the research objective were excluded using a screening tool (Additional file 3: Search Tool). First, the titles and abstracts of publications were screened to determine if studies conducted quantitative surveys, and to assess if self-reported and/or proxy-reported OHS was a primary objective. Only surveys with more than three questions that related to OHS were considered. Studies with secondary analysis were excluded because the data collection methods were normally not developed as part of the research and were developed previously. Papers whose sole purpose was to validate well-known measures of oral health were also rejected since the intent was not to assess the OHS of a population. Literature reviews were likewise excluded, as were papers describing results from focus groups and other qualitative studies. Papers whose objectives were to validate measures or predict specific oral disease entities, such as caries or gingival bleeding, rather than overall OHS. Studies primarily focusing on general health status or other systemic diseases instead of OHS were eliminated. Randomized Controlled Trials (RCT) or quasi RCT studies that tested an active agent (e.g., therapy, experiment, and medicine) were excluded because the main research purpose was a comparison of treatment rather than an assessment of subject-reported OHS.
The research team performed the secondary screening through a full-text review. We dropped papers with full text missing or not in English. Then, we screened the available full-text works using a similar set of inclusion criteria aforementioned and further excluded papers without information about data collection methods.
Selection strategies
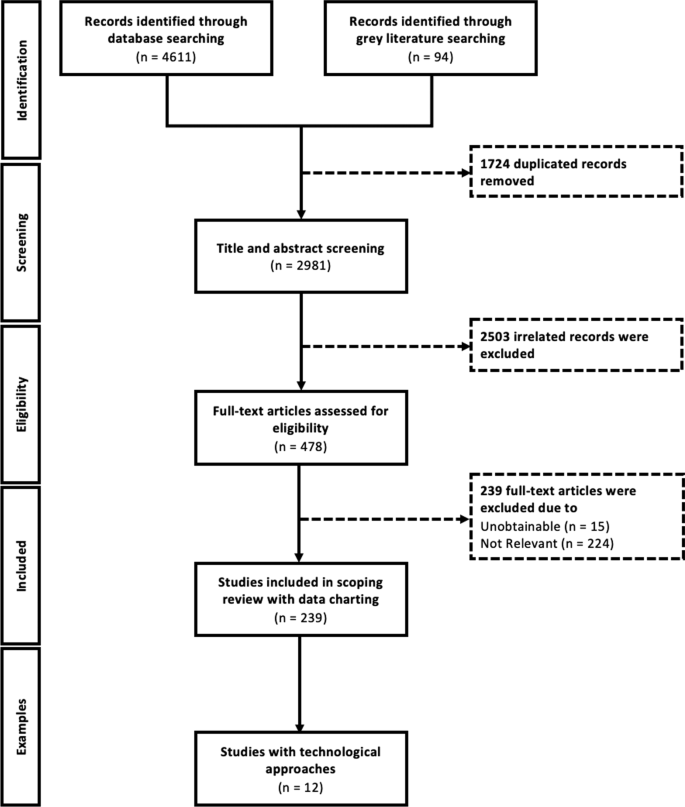
Figure 1 outlines the review process utilizing the PRISMA-ScR framework. The title-and-abstract screening was completed by a researcher (D.X.) against the inclusion criteria using a screening tool (Additional file 3: Search Tool). To check for reliability and consistency, one of the researchers (L.Z.) randomly screened 10% of articles independently and compared the inclusion decisions. Given the result of title-and-abstract screening, two researchers (L.Z. and Y.H.) verified the eligibility of the remaining articles independently through full-text review. Inclusion discrepancies were resolved by an additional researcher (D.X.).
Data extraction
The data charting form (Additional file 4: Data Charting Form) consists of quantitative and qualitative variables for the data collection methods and their characteristics, such as outcome measures, use of assistive devices/tools or data sources, report type, and so on. The form has been pre-tested by two project staff (C.M. and M.M.) before being utilized. Two researchers (Y.H. and L.Z.) extracted data using the form. Two project staff (C.M. and M.M.) collaborated to review the charted study characteristics and the discrepancies have been addressed through discussion.
Data synthesis and analysis
The scoping review synthesizes the research findings based on dimensions and attributes of major oral health survey data collection methods using descriptive and content analyses. The review provides an overview of various related data collection methods in the recent literature, which refer to the quantitative methods to collect information from a pool of respondents, and the trends in using these new technological approaches, which involve computerized modes, Internet-supported devices and interactive web technologies. Through the literature review, we locate four major types of data collection methods: in-person, Internet-based, telephone-based, and mail-in based approaches.
Results
Screening and study selection
After removing duplicates, the initial search revealed 2981 articles from four online databases for title-and-abstract screening; 2503 of which were excluded after being examined against the inclusion criteria. The interrater reliability of screening was measured by Kappa agreement as 0.94 (95% confidence interval [0.89, 0.99]) for title-and-abstract screening, which implies almost perfect agreement [21]. After full-text reviewing and excluding 239 articles, we summarized and categorized the remaining 239 studies based on the pre-tested data charting form. In addition, we identified 12 studies with various technological approaches to data collection. Figure 1 presented the PRISMA Framework used for this scoping review.
General characteristics of included studies
Table 1 presents various characteristics of the 239 articles that meet inclusion criteria that were published from 2011 to September 2021. Fifty-six percent of the papers are published in dental journals. About 40% of the papers are published in journals from the Asia-Pacific and Middle East region (APAC), and only 8.4% are from North America (NA). The majority of studies (69%) focus on the general population. Most (88.6%) of the studies use in-person surveys. Around two-thirds of the studies invite and recruit participants from the study sites, e.g., schools, clinics, and hospitals. Some studies recruit participants by having the research team visit communities (16%) or by sampling directly from a database (13%). In the latter case, participants are selected using probability and/or non-probability sampling methods, including convenience sampling (52%), simple random sampling (12%), and stratified sampling (12%). Most studies (193 or 80.8%) investigate self-reported outcomes. Dental examinations accompany the survey in 54% of the studies, while 32% of studies do not use any clinical exam or records. The data charting details are listed in Additional file 4: Data Charting Form.
Characteristics of data collection methods
The four main data collection methods include in-person (N = 206, 86.2%), mail-in (N = 15, 6.3%), Internet-based (N = 6, 2.5%), and telephone-based (N = 3, 1.3%) surveys. The characteristics of the various data collection methods are summarized in Table 2.
The majority of the studies using in-person surveys have high response rates with an average of 90.6%. Those studies using in-person survey methods represent half 55.8% of the studies employ face-to-face interviews, while 35.4% used a paper-and-pencil approach. Participants for 58.7% of the studies are recruited directly from clinics [22], hospitals [23], and community care centers [24]. For those sites with electronic records, additional data sources are directly linked to the survey, for example, clinical dental exams with visual components (e.g., X-ray [25] and pictures [26]) and medical records [23, 27, 28]. Moreover, different qualitative assessments (e.g., Malocclusion Assessment [22] and Masticatory Performance Test [24, 29]) are captured in patient progress notes.
The mail-in survey method is used by 15 studies and may be more cost-effective than in-person delivery, though these were the two main sources, via post (80%) and by carriers (20%). Mail-in surveys have a relatively high response rate averaging 72%, especially when children or other respondents bring surveys home to complete. Similar to in-person surveys, mail-in surveys can incorporate additional resources, such as photographs and explanations of clinical conditions and treatments [30, 31].
Only six studies are identified as using an Internet-based survey, mainly through computer-assisted web interviews (4 studies), and email (2 studies). Three papers employ direct recruitment and another three papers recruit participants through websites and databases. The average response rate is as low as 36.7% for this method with small sample sizes with a median of 259 participants.
Three studies use a telephone survey method covering large populations compared to other survey methods with more responders on average. Two of these studies recruit participants through an existing database, and all surveys used interviewers. Computer-Assisted Telephone Interviews (CATI) [32] and Voice Response Systems [33] which are commonly used in industry are not found in the studies.
In addition to the data collection methods, we further categorize the measures found in the 239 articles. Table 3 presents the frequencies and percentages of the various self-reported outcome measures. The three basic approaches are oral health impact measures [34], functional measures [34], and self- or proxy-ratings of OHS, with the terms defined in Additional file 5: Glossary of Terms. These are used as single measures or in combination. The Oral Health Impact Profile-14 (OHIP-14) is the most prevalent single measure with 69 papers and 29% overall, of which 25 papers are about child impact, representing 10% of the total number of selected papers. The Geriatric Oral Health Assessment Index (GOHAI), a functional measure, is second with 21 papers and 9% overall. The GOHAI is the first among the studies on the elderly. There are also two adolescent papers representing 9% of the functioning category. The self- or proxy-rating of OHS has 18 single-measure papers representing 8% of these articles. Of these, 12 or 80% are children's measure's, representing 5% of all selected papers.
There is a total of 63 papers using more than one type of measure. Either combining functional and impact measures (36 and 15%) or self-rating OHS and one or more of the other measures (27 or 11%). The group of single impact measures is 50% of the overall and also represents where two or more measures were used. The single measure, GOHAI, based on function is only 9% of all measures but also played a role in combination with other measures. Finally, the self-reported OHS as a single measure represents 8% of the studies. Its role is mainly in combination with other measures and represented another 15% of the articles. In total. children's oral health measures form a considerable portion of the self-reported oral health outcome research papers, representing 16% of all studies. There are additional studies where children’s measures are used in combination with adults.
Currently, the use of technological approaches emerged in the field of survey research to improve the quality and quantity of data collection. After reviewing and charting all qualified 239 articles, twelve studies that employ technological approaches are summarized in Table 4.
Discussion
This scoping review provides an overview of data collection methods used for subject-reported surveys to measure oral health outcomes. Studies are characterized by four survey methods (in-person, mail-in, Internet-based, and telephone) and by summarized dimensions and attributes of data collection for each method, such as technological approaches, survey population or sampling methods. Studies typically employ in-person surveys and more studies were conducted in Asia-Pacific and Middle East countries than in any other world region. Most studies recruit participants directly from study sites. Both probability and non-probability sampling methods employ typically convenience sampling, simple random sampling, and stratified sampling. Studies that achieve the highest response rate on average use in-person surveys, while the lowest rate occurs in Internet-based surveys. Telephone surveys are used to cover a wider population compared to other data collection methods. Many studies, especially those using in-person and mail-in data collection methods, incorporate supplemental data types and technological approaches. Outcome measures are frequently used to evaluate impacts caused by functional limitations related to physical, psychological, and social factors.
Frequently used self-reported oral health status and OHRQoL measures are OHIP-14, an impact measure, and the GOHAI, a functional measure. Children’s oral health outcomes measures form a considerable portion of the self-reported oral health outcome research papers. Although OHIP-14 is the most utilized single measure, many other papers use only portions of this measure, while adding other outcome measures, such as dental care needs, satisfaction, oral health status, and so on. The validity of these measures is therefore compromised and could not provide insight into the degree that the studies are measuring self-reported oral health status or quality of life [4]. Other measures rate an individual’s oral health status using a simple self-rating scale, from very poor to excellent. This approach is more directly related to a person’s oral conditions and therefore their perceptions and behavior tend to be more consistent with this rating [56, 57]. These self-rating measures focus on the overall dimension of perceived oral health status. Unlike the measures previously discussed, these simple ratings do not delineate the psychological, social and physical dimensions of oral health. Nevertheless, such measures can enable researchers to identify hidden dimensions by analyzing independent variables that account for the respondent’s perception.
This review identifies research that employs more conventional methods. The face-to-face interview and the pencil and paper format are conventionally used in many studies along with a clinical dental exam. While offering unique flexibility and easier administration, in-person approaches are more labor-intensive and normally take more time compared to other methods. Countries, such as Brazil, rely for years on these techniques to develop national epidemiological oral health surveys [28, 58, 59]. Although these surveys are very well-organized and established throughout the country, this review does not find that newer technological approaches are introduced into their conventional approach. In this case, there may be little incentive to change their approach because their methods are well understood and employing more technological approaches may be costly.
The use of Internet-based surveys is increasingly common in the medical field. Although these surveys end with potentially lower response rates, this approach is normally more cost-effective [60]. Internet-based surveys have many notable advantages, including easy administration, fast data collection process, lower cost, wider population coverage and better data quality with fewer overall data errors and fewer missing items [61,62,63]. However, this data collection method is constrained by sample bias, topic salience, data security concerns and low digital literacy that may affect response rates [62]. In settings where Internet-based surveys are not practical, longstanding and effective conventional oral health data collection methods in research will continue. It is evident from this review that the use of computerized technological approaches is limited. While such approaches in survey research improve the quality and quantity of data collection, only twelve studies in this review employ them. The most widely used technical approaches are Computer-Assisted Personal Interviewing (CAPI) and online survey platforms (e.g., Google Forms and SurveyMonkey).
Two noteworthy approaches to survey research methodology emerge from this review, particularly in: (1) sample selection, and (2) mode of interaction with research subjects. North American researchers found different platforms to access subjects for their studies. Canadian studies use random digit dialing to recruit and conduct computer-assisted interviews [54]. In the United States, researchers access existing polling populations or use Amazon’s MTurk platform for “workers” who are paid small amounts for each survey they respond to [64]. The second approach is the use of computers to collect self-reported data. The basic surveying technique is CAPI with interviewers directly entering the data into a database. There is also Computer-Assisted Telephone Interviewing (CATI), a survey technique, where the interviewer follows a scripted interview guided by a questionnaire that appears on the screen. A third Internet-based survey technique, the Computer-Assisted Web Interviewing (CAWI), requires no live interviewer. Instead, the respondent follows a script made in a program for designing web interviews that may include images, audio and video clips, and web-based information.
An innovative technological approach worth noting is the use of OralCam to perform self-examination using a smartphone camera [65]. The study applies research used in medicine to detect liver problems from face photos as well as other diseases [66]. The paper describes the use of a smartphone camera to interact with a computer using diagnostic algorithms, such as the deep convolutional neural network-based multitask learning approach. Based on over three thousand intraoral photos, the system learns to analyze teeth and gingiva. The smartphone camera takes a picture using a mouth opener. The computer’s algorithms analyze the captured picture, along with survey data, to diagnose several dental conditions including caries, chronic gingival inflammation, and dental calculus. This use of multitask learning technology, with the extensive availability of cell phones, may revolutionize oral health research and care.
This scoping review is limited to oral health survey-based studies in peer-reviewed journals and MedRxiv published in English between 2011 to 2021. A further limitation is that many of the reviewed papers do not adequately describe the methods they use to collect data. Publications using secondary data from national studies are excluded, The exclusion is based on the fact that these researchers are not engaged in designing the methods or conducting the data collection. Often, the publications refer to the original study to describe the method used. Also, the original data collection may have occurred before the time frame of this review. The fifteen papers that use secondary data published over this study’s time frame represent only about six percent of the reviewed papers. Thus, the overall impact of this exclusion is minimal on this scoping review’s results.
Conclusions
This scoping review provides an assessment of oral health outcome measures, including subject-reported oral health status, and notes newly emerging computer technological approaches recently used in surveys conducted on general populations. Such technological approaches, although rarely used in the reviewed studies, hold promise for both researchers and the various populations that use or need oral health care. Future studies employing more developed computer applications for survey research to boost recruitment and participation of study subjects with wide and diverse backgrounds from almost unlimited geographic areas can then provide a broader perspective on oral health survey methods and outcomes.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- PRISMA-ScR:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews
- APAC:
-
Asia-Pacific (including the Middle East)
- EUR:
-
Europe
- LATAM:
-
Latin America
- NA:
-
North America
- AFR:
-
Africa
- CAPI:
-
Computer-Assisted Personal Interviewing
- CAWI:
-
Computer-Assisted Web Interviewing
- CATI:
-
Computer-Assisted Telephone Interview
- OHRQoL:
-
Oral Health-Related Quality of Life
- OHIP-14:
-
Oral Health Impact Profile-14
- GOHAI:
-
Geriatric Oral Health Assessment Index
- OHS:
-
Oral Health Status
References
Watt RG, Daly B, Allison P, Macpherson LMD, Venturelli R, Listl S, et al. Ending the neglect of global oral health: time for radical action. Lancet. 2019;394:261–72. https://doi.org/10.1016/S0140-6736(19)31133-X.
Liu H, Hays R, Wang Y, Marcus M, Maida C, Shen J, et al. Short form development for oral health patient-reported outcome evaluation in children and adolescents. Qual Life Res. 2018;27:1599–611. https://doi.org/10.1007/S11136-018-1820-9.
Wang Y, Hays R, Marcus M, Maida C, Shen J, Xiong D, et al. Development of a parents’ short form survey of their children’s oral health. Int J Pediatr Dent. 2019;29:332–44. https://doi.org/10.1111/ipd.12453.
Yang C, Crystal YO, Ruff RR, Veitz-Keenan A, McGowan RC, Niederman R. Quality appraisal of child oral health-related quality of life measures: a scoping review. JDR Clin Transl Res. 2020;5:109–17. https://doi.org/10.1177/2380084419855636.
Gupta M, Bosma H, Angeli F, Kaur M, Chakrapani V, Rana M, et al. A mixed methods study on evaluating the performance of a multi-strategy national health program to reduce maternal and child health disparities in Haryana. India BMC Public Health. 2017;17:698. https://doi.org/10.1186/s12889-017-4706-9.
Keboa MT, Hiles N, Macdonald ME. The oral health of refugees and asylum seekers: a scoping review. Glob Health. 2016;12:1–11. https://doi.org/10.1186/S12992-016-0200-X/TABLES/2.
Wilson NJ, Lin Z, Villarosa A, Lewis P, Philip P, Sumar B, et al. Countering the poor oral health of people with intellectual and developmental disability: a scoping literature review. BMC Public Health. 2019;19:1–16. https://doi.org/10.1186/S12889-019-7863-1/TABLES/1.
Ajwani S, Jayanti S, Burkolter N, Anderson C, Bhole S, Itaoui R, et al. Integrated oral health care for stroke patients—a scoping review. J Clin Nurs. 2017;26:891–901. https://doi.org/10.1111/JOCN.13520.
Shrestha AD, Vedsted P, Kallestrup P, Neupane D. Prevalence and incidence of oral cancer in low- and middle-income countries: a scoping review. Eur J Cancer Care. 2020;29:66. https://doi.org/10.1111/ECC.13207.
Patterson-Norrie T, Ramjan L, Sousa MS, Sank L, George A. Eating disorders and oral health: a scoping review on the role of dietitians. J Eat Disord. 2020;8:1–21. https://doi.org/10.1186/S40337-020-00325-0/TABLES/1.
Lansdown K, Smithers-Sheedy H, Mathieu Coulton K, Irving M. Oral health outcomes for people with cerebral palsy: a scoping review protocol. JBI Database System Rev Implement Rep 2019;17:2551–8. https://doi.org/10.11124/JBISRIR-2017-004037.
Beaton L, Humphris G, Rodriguez A, Freeman R. Community-based oral health interventions for people experiencing homelessness: a scoping review. Community Dent Health. 2020;37:150–60. https://doi.org/10.1922/CDH_00014BEATON11.
Marquillier T, Lombrail P, Azogui-Lévy S. Social inequalities in oral health and early childhood caries: How can they be effectively prevented? A scoping review of disease predictors. Rev Epidemiol Sante Publique. 2020;68:201–14. https://doi.org/10.1016/J.RESPE.2020.06.004.
Como DH, Duker LIS, Polido JC, Cermak SA. The persistence of oral health disparities for African American children: a scoping review. Int J Environ Res Public Health. 2019;16:66. https://doi.org/10.3390/IJERPH16050710.
Stein K, Farmer J, Singhal S, Marra F, Sutherland S, Quiñonez C. The use and misuse of antibiotics in dentistry: a scoping review. J Am Dent Assoc. 2018;149:869-884.e5. https://doi.org/10.1016/J.ADAJ.2018.05.034.
Mittal H, John MT, Sekulić S, Theis-Mahon N, Rener-Sitar K. Patient-reported outcome measures for adult dental patients: a systematic review. J Evid Based Dent Pract. 2019;19:53–70. https://doi.org/10.1016/J.JEBDP.2018.10.005.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method Theory Pract. 2005;8:19–32. https://doi.org/10.1080/1364557032000119616.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. https://doi.org/10.1186/1748-5908-5-69.
Paré G, Trudel M-C, Jaana M, Kitsiou S. Synthesizing information systems knowledge: a typology of literature reviews. Inf Manag. 2015. https://doi.org/10.1016/j.im.2014.08.008.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73. https://doi.org/10.7326/M18-0850.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159. https://doi.org/10.2307/2529310.
Masood M, Masood Y, Newton T, Lahti S. Development of a conceptual model of oral health for malocclusion patients. Angle Orthod. 2015;85:1057–63. https://doi.org/10.2319/081514-575.1.
Massarente DB, Domaneschi C, Marques HHS, Andrade SB, Goursand D, Antunes JLF. Oral health-related quality of life of paediatric patients with AIDS. BMC Oral Health. 2011;11:2. https://doi.org/10.1186/1472-6831-11-2.
Lu TY, Chen JH, Du JK, Lin YC, Ho PS, Lee CH, et al. Dysphagia and masticatory performance as a mediator of the xerostomia to quality of life relation in the older population. BMC Geriatr. 2020;20:66. https://doi.org/10.1186/S12877-020-01901-4.
Strömberg E, Holmèn A, Hagman-Gustafsson ML, Gabre P, Wardh I. Oral health-related quality-of-life in homebound elderly dependent on moderate and substantial supportive care for daily living. Acta Odontol Scand. 2013;71:771–7. https://doi.org/10.3109/00016357.2012.734398.
Morgan JP, Isyagi M, Ntaganira J, Gatarayiha A, Pagni SE, Roomian TC, et al. Building oral health research infrastructure: the first national oral health survey of Rwanda. Glob Health Act. 2018;11:66. https://doi.org/10.1080/16549716.2018.1477249.
Preciado A, del Río J, Suárez-García MJ, Montero J, Lynch CD, Castillo-Oyagüe R. Differences in impact of patient and prosthetic characteristics on oral health-related quality of life among implant-retained overdenture wearers. J Dent. 2012;40:857–65. https://doi.org/10.1016/J.JDENT.2012.07.006.
de Quadros Coelho M, Cordeiro JM, Vargas AMD, de Barros Lima Martins AME, de Almeida Santa Rosa TT, Senna MIB, et al. Functional and psychosocial impact of oral disorders and quality of life of people living with HIV/AIDS. Qual Life Res. 2015;24:503–11. https://doi.org/10.1007/S11136-014-0778-5.
Said M, Otomaru T, Aimaijiang Y, Li N, Taniguchi H. Association between masticatory function and oral health-related quality of life in partial maxillectomy patients. Int J Prosthodont. 2016;29:561–4. https://doi.org/10.11607/IJP.4852.
Owens J, Jones K, Marshman Z. The oral health of people with learning disabilities—a user–friendly questionnaire survey. Community Dent Health. 2017;34:4–7. https://doi.org/10.1922/CDH_3867OWENS04.
Abuzar MA, Kahwagi E, Yamakawa T. Investigating oral health-related quality of life and self-perceived satisfaction with partial dentures. J Investig Clin Dent. 2012;3:109–17. https://doi.org/10.1111/J.2041-1626.2012.00111.X.
Wilson D, Taylor A, Chittleborough C. The second Computer Assisted Telephone Interview (CATI) Forum: the state of play of CATI survey methods in Australia. Aust NZ J Public Health. 2001;25:272–4. https://doi.org/10.1111/J.1467-842X.2001.TB00576.X.
Lee H, Friedman ME, Cukor P, Ahern D. Interactive voice response system (IVRS) in health care services. Nurs Outlook. 2003;51:277–83. https://doi.org/10.1016/S0029-6554(03)00161-1.
Campos JADB, Zucoloto ML, Bonafé FSS, Maroco J. General Oral Health Assessment Index: a new evaluation proposal. Gerodontology. 2017;34:334–42. https://doi.org/10.1111/GER.12270.
Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. https://doi.org/10.1111/J.1600-0528.1997.TB00941.X.
Adulyanon S, Vourapukjaru J, Sheiham A. Oral impacts affecting daily performance in a low dental disease Thai population. Community Dent Oral Epidemiol. 1996;24:385–9. https://doi.org/10.1111/J.1600-0528.1996.TB00884.X.
Pahel BT, Rozier RG, Slade GD. Parental perceptions of children’s oral health: the Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual Life Outcomes. 2007;5:6. https://doi.org/10.1186/1477-7525-5-6.
Gherunpong S, Tsakos G, Sheiham A. Developing and evaluating an oral health-related quality of life index for children: the CHILD-OIDP. Undefined. 2004;21:161–9.
Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11.
Broder HL, Wilson-Genderson M. Reliability and convergent and discriminant validity of the Child Oral Health Impact Profile (COHIP Child’s version). Community Dent Oral Epidemiol. 2007;35(Suppl 1):20–31. https://doi.org/10.1111/J.1600-0528.2007.0002.X.
Atieh MA. Arabic version of the geriatric oral health assessment Index. Gerodontology. 2008;25:34–41. https://doi.org/10.1111/j.1741-2358.2007.00195.x.
Wright WG, Spiro A, Jones JA, Rich SE, Garcia RI. Development of the teen oral health-related quality of life instrument. J Public Health Dent. 2017;77:115–24. https://doi.org/10.1111/JPHD.12181.
Jokovic A, Locker D, Tompson B, Guyatt G. Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. Undefined. 2004;26:512–8.
Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81:459–63. https://doi.org/10.1177/154405910208100705.
Broughton JR, TeH Maipi J, Person M, Randall A, Thomson WM. Self-reported oral health and dental service-use of rangatahi within the rohe of Tainui. NZ Dent J. 2012;108:90–4.
Monaghan N, Karki A, Playle R, Johnson I, Morgan M. Measuring oral health impact among care home residents in Wales. Community Dent Health. 2017;34:14–8. https://doi.org/10.1922/CDH_3950MORGAN05.
Echeverria MS, Silva AER, Agostini BA, Schuch HS, Demarco FF. Regular use of dental services among university students in southern Brazil. Revista de Saude Publica 2020;54:85. https://doi.org/10.11606/S1518-8787.2020054001935.
Mohamad Fuad MA, Yacob H, Mohamed N, Wong NI. Association of sociodemographic factors and self-perception of health status on oral health-related quality of life among the older persons in Malaysia. Geriatr Gerontol Int. 2020;20(Suppl 2):57–62. https://doi.org/10.1111/GGI.13969.
Hanisch M, Wiemann S, Bohner L, Kleinheinz J, Susanne SJ. Association between oral health-related quality of life in people with rare diseases and their satisfaction with dental care in the health system of the Federal Republic of Germany. Int J Environ Res Public Health. 2018. https://doi.org/10.3390/IJERPH15081732.
Nam SH, Kiml HY, IlChun D. Influential factors on the quality of life and dental health of university students in a specific area. Biomed Res. 2017;28:12.
Mortimer-Jones S, Stomski N, Cope V, Maurice L, Théroux J. Association between temporomandibular symptoms, anxiety and quality of life among nursing students. Collegian. 2019;26:373–7. https://doi.org/10.1016/J.COLEGN.2018.10.003.
Liu C, Zhang S, Zhang C, Tai B, Jiang H, Du M. The impact of coronavirus lockdown on oral healthcare and its associated issues of pre-schoolers in China: an online cross-sectional survey. BMC Oral Health. 2021;21:66. https://doi.org/10.1186/s12903-021-01410-9.
Makizodila BAM, van de Wijdeven JHE, de Soet JJ, van Selms MKA, Volgenant CMC. Oral hygiene in patients with motor neuron disease requires attention: a cross-sectional survey study. Spec Care Dent. 2021. https://doi.org/10.1111/SCD.12636.
Kotzer RD, Lawrence HP, Clovis JB, Matthews DC. Oral health-related quality of life in an aging Canadian population. Health Qual Life Outcomes. 2012;10:50. https://doi.org/10.1186/1477-7525-10-50.
Hakeberg M, Wide U. General and oral health problems among adults with focus on dentally anxious individuals. Int Dent J. 2018;68:405–10. https://doi.org/10.1111/IDJ.12400.
Lawal FB, Olawole WO, Sigbeku OF. Self rating of oral health status by student dental surgeon assistants in Ibadan, Nigerian—a Pilot Survey. Ann Ibadan Postgrad Med. 2013;11:12.
Locker D, Wexler E, Jokovic A. What do older adults’ global self-ratings of oral health measure? J Public Health Dent. 2005;65:146–52. https://doi.org/10.1111/J.1752-7325.2005.TB02804.X.
Saintrain MVDL, de Souza EHA. Impact of tooth loss on the quality of life. Gerodontology. 2012;29:66. https://doi.org/10.1111/J.1741-2358.2011.00535.X.
Grando LJ, Mello ALSF, Salvato L, Brancher AP, del Moral JAG, Steffenello-Durigon G. Impact of leukemia and lymphoma chemotherapy on oral cavity and quality of life. Spec Care Dent. 2015;35:236–42. https://doi.org/10.1111/SCD.12113.
Ebert JF, Huibers L, Christensen B, Christensen MB. Paper- or Web-Based Questionnaire Invitations as a method for data collection: cross-sectional comparative study of differences in response rate, completeness of data, and financial cost. J Med Internet Res. 2018;20:66. https://doi.org/10.2196/JMIR.8353.
Hohwü L, Lyshol H, Gissler M, Jonsson SH, Petzold M, Obel C. Web-based versus traditional paper questionnaires: a mixed-mode survey with a Nordic perspective. J Med Internet Res. 2013;15:66. https://doi.org/10.2196/JMIR.2595.
Maymone MBC, Venkatesh S, Secemsky E, Reddy K, Vashi NA. Research techniques made simple: Web-Based Survey Research in Dermatology: conduct and applications. J Invest Dermatol. 2018;138:1456–62. https://doi.org/10.1016/J.JID.2018.02.032.
Weigold A, Weigold IK, Natera SN. Response rates for surveys completed with paper-and-pencil and computers: using meta-analysis to assess equivalence. Soc Sci Comput Rev. 2018;37:649–68. https://doi.org/10.1177/0894439318783435.
Burnham MJ, Le YK, Piedmont RL. Who is Mturk? Personal characteristics and sample consistency of these online workers. Ment Health Relig Cult. 2018;21:934–44. https://doi.org/10.1080/13674676.2018.1486394.
Liang Y, Fan HW, Fang Z, Miao L, Li W, Zhang X, et al. OralCam: enabling self-examination and awareness of oral health using a smartphone camera. In: Conference on human factors in computing systems—proceedings, vol 20. New York: Association for Computing Machinery; 2020. p. 1–13. https://doi.org/10.1145/3313831.3376238.
Ding X, Jiang Y, Qin X, Chen Y, Zhang W, Qi L. Reading face, reading health: Exploring face reading technologies for everyday health. In: Conference on human factors in computing systems—proceedings. New York: Association for Computing Machinery; 2019. p. 1–13. https://doi.org/10.1145/3290605.3300435.
Acknowledgements
Not applicable.
Funding
This research was supported by an NIDCR/NIH grant to the University of California, Los Angeles (UCLA) (U01DE029491). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
C.M., D.X., M.M. and H.L. conceptualized the study and designed the data collection form and established the data analysis plan. A.O. developed search strategies and carried out searching on multiple databases. D.X., Y.L., Y.H., J.S. and Y.L. performed additional searching and tested the data charting form. D.X., Y.L., and Y.H. helped to screen studies for relevance and data charting. C.M. and M.M. reviewed full-text papers and verify the data charting results. C.M., D.X., and M.M. drafted the original manuscript. D.X. and L.Z. prepared Tables 1, 2 and Fig. 1. C.M., D.X., M.M., and L.Z prepared Tables 3 and 4. All authors read and provided substantial comments/edits on the manuscript and approved the final version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Additional file 2.
Search Terms.
Additional file 3.
Search Tool.
Additional file 4.
Data Charting Form.
Additional file 5.
Glossary of Terms.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Maida, C.A., Xiong, D., Marcus, M. et al. Quantitative data collection approaches in subject-reported oral health research: a scoping review. BMC Oral Health 22, 435 (2022). https://doi.org/10.1186/s12903-022-02399-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-022-02399-5